NVA Lustrum Congres 2025
-
Waar:
Grand Hotel Huis ter Duin
Kon. Astrid Boulevard 5
2202 BK
Noordwijk
Nederland -
Wanneer:
04/09/2025 - 05/09/2025
08:30 - 17:30 -
Accreditatie door:
NOV, VSG en Kwaliteitsregister Fysiotherapie met 12 punten
Heeft u een vraag over dit event?
Neem contact met ons op!Telefoon: 013-5440013 Email: info@excelcs.nl
Veelgestelde vragen
-
Het lukt me niet om mezelf in te schrijven.
Heeft u het registratieformulier volledig ingevuld, maar verschijnt de donkerblauwe button onderaan met ‘inschrijven’ niet of klikt u op ‘inschrijven’ en krijgt u de volgende melding: ‘There was a problem with your submission. Please review the fields below’, dan vragen we u de volgende items in uw registratie na te kijken:
Heeft u uw geslacht ingevuld?
Heeft u uw e-mailadres twee keer ingevuld?
Bent u akkoord gegaan met de annulerings- en wijzigingsvoorwaarden?
Mocht u vervolgens de volgende melding krijgen:
Dit e-mailadres is al geregistreerd
Dan betekent dat, dat u zich al eens eerder via onze website voor een (ander) congres heeft geregistreerd en toen reeds een ‘account’ op onze website heeft aangemaakt. Het systeem ‘kent’ u daarom al. Dit betekent echter NIET dat u voor dit congres ingeschreven staat. Wanneer u helemaal onderaan het formulier het vakje UIT vinkt bij de volgende vraag: Wil je direct ook een account aanmaken zodat het inschrijven vervolgens vele malen sneller gaat? Dan kunt u zich wel registreren.
Heeft u bovenstaande acties goed uitgevoerd maar kunt u zich nog steeds niet inschrijven? Mail dan naar info@excelcs.nl.
-
Ik heb geen bevestiging ontvangen van mijn inschrijving.
Het kan zijn dat de bevestiging in uw spam of ongewenste mail terecht is gekomen. De factuur ontvangt u in een aparte e-mail. Als dit niet het geval is, kunt u mailen naar info@excelcs.nl.
-
Ik heb geen factuur ontvangen.
Het kan zijn dat de factuur in uw spam of ongewenste mail terecht is gekomen. Als dit niet het geval is, kunt u mailen naar info@excelcs.nl.
- Over
- Over NVA
- Programma
- Speakers - Sept. 4th
- Speakers - Sept. 5th
- Call for abstracts
- Locatie
- Registratie-tarieven
- Inschrijven
- Sponsoring
Over het NVA Lustrum Congres 2025
Op donderdag 4 en vrijdag 5 september 2025 vindt het NVA Lustrum Congres 2025 plaats. De NVA bestaat dan 35 jaar!
Deze bijeenkomst organiseren wij voor de Nederlandse Vereniging voor Arthroscopie (NVA), bedoelt voor iedereen, zowel leden als niet-leden van de NVA, met interesse in dit vakgebied. Het congres wordt samengesteld uit diverse actuele onderwerpen binnen de arthroscopische chirurgie.
Accreditatie is toegekend door VSG en Kwaliteitsregister Fysiotherapie met 12 punten, door NOV met 9 punten.
Promotie actie – Bring Your Own Sportsmed / Sportsfysio
Kent u of werkt u samen met een sportmedische arts of fysiotherapeut die dit ook niet wil missen? Introduceer deze persoon en ontvang beiden €50,- korting op de tickets. Hoe werkt dit? Schrijf u beiden in voor het congres, voeg de naam van deze persoon toe bij de daarvoor bestemde vraag. Gebruik de kortingscode: promonva25 in het kopje vóór betaling. Zo kunnen jullie dit samen beleven!
Over de NVA (Nederlandse Vereniging voor Arthroscopie)
De Nederlandse Vereniging voor Arthroscopie is in 1990 opgericht. Het is en vereniging voor en door jonge, dynamische (orthopedisch) chirurgen. De NVA heeft als doel het verbeteren van de arthroscopische kennis en kunde. Om dit doel te bereiken organiseert de NVA jaarlijks een jaarcongres, een 6-tal hands on scopiecursussen (oplopend in moeilijkheidsgraad), een masterclass en een aantal fellowships.
Meer weten over de NVA? Kijk op https://scopie.org/
Wilt u meer informatie over een NVA lidmaatschap? Klik dan hier!
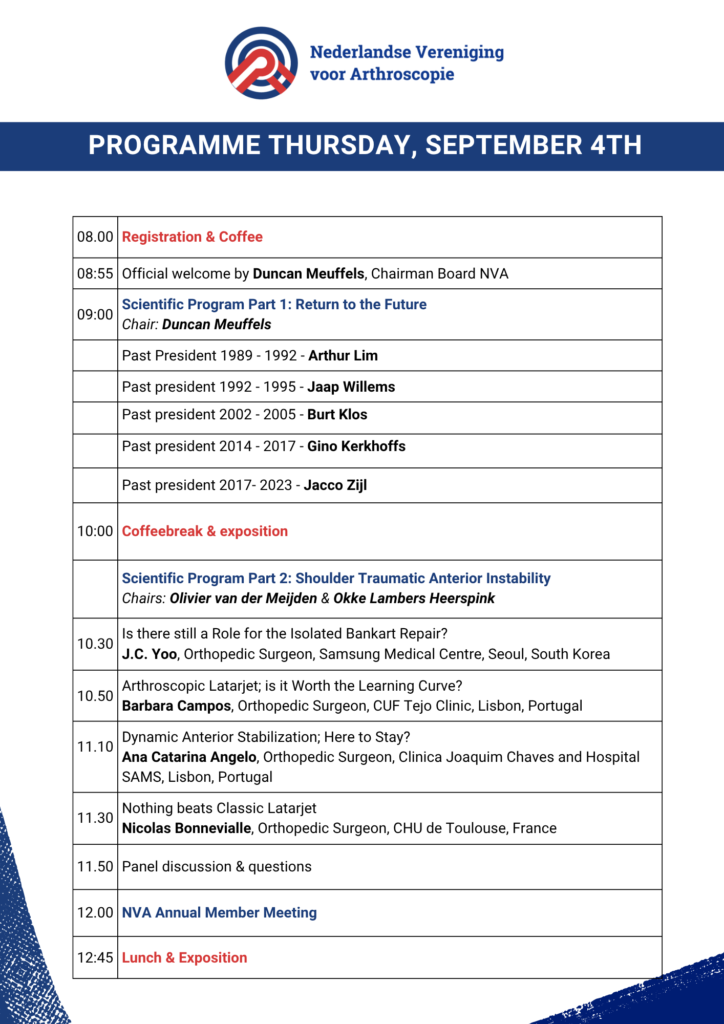
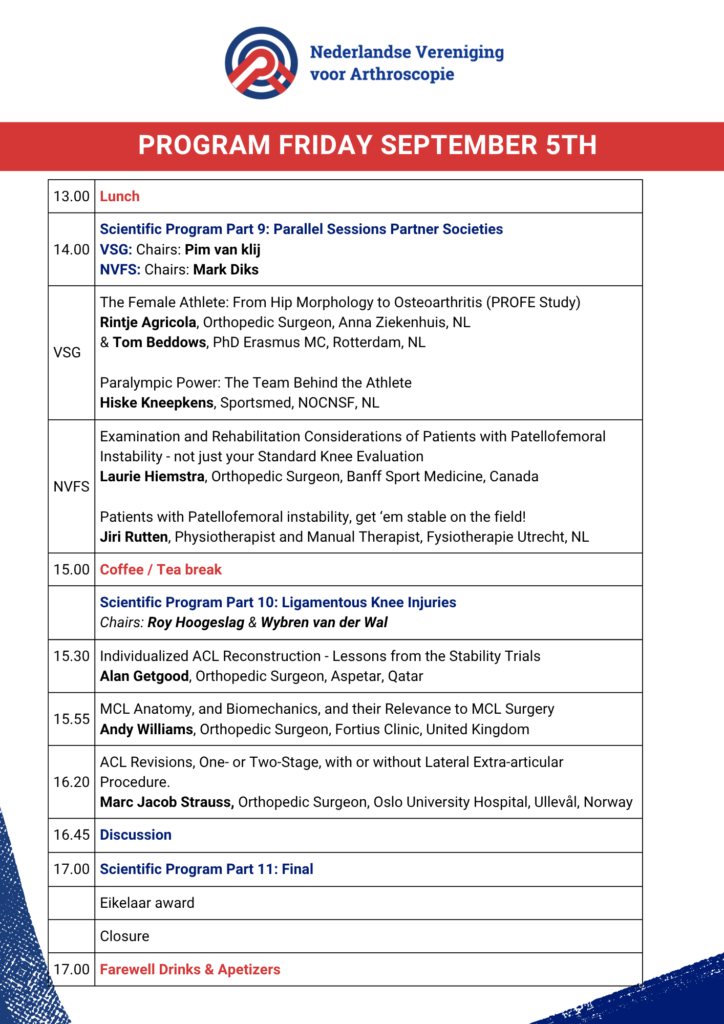
Programme





J.C. Yoo
Orthopedic Surgeon, Samsung Medical Centre, Seoul, South Korea
Is there still a Role for the Isolated Bankart Repair?
In recent years, the management of anterior shoulder instability has evolved significantly, raising questions about the continued relevance of the isolated Bankart repair. In this lecture, Dr. J.C. Yoo explores the current indications, outcomes, and limitations of the isolated Bankart procedure in comparison to alternative surgical techniques such as the Latarjet procedure and remplissage. Drawing on clinical experience and recent evidence, Dr. Yoo discusses patient selection criteria, recurrence rates, and biomechanical considerations. The presentation aims to clarify whether and when an isolated Bankart repair remains a viable option in modern orthopedic practice.
Barbara Campos
Orthopedic Surgeon, CUF Tejo Clinic, Lisbon, Portugal
Arthroscopic Latarjet; is it worth the learning curve?
The arthroscopic Latarjet procedure has gained popularity as a minimally invasive alternative for treating anterior shoulder instability with significant bone loss. However, the technical complexity and steep learning curve remain barriers to widespread adoption. In this lecture, Dr. Barbara Campos critically examines whether the potential benefits of the arthroscopic approach—such as reduced soft tissue damage, improved visualization, and faster recovery—justify the time and effort required to master the technique. Drawing on current literature, surgical experience, and outcome data, this talk provides practical insights into patient selection, complication rates, and the role of arthroscopic Latarjet in comparison to open procedures. The session will be especially valuable for surgeons considering the transition to this advanced technique.
Ana Catarina Angelo
Orthopedic Surgeon, Clinica Joaquim Chaves and Hospital SAMS, Lisbon, Portugal
‘Dynamic Anterior Stabilisation; here to stay?’
The surgical treatment of glenohumeral anteroinferior instability in shoulders with limited to subcritical glenoid bone loss remains a controversial subject. The Dynamic Anterior Stabilization (DAS) technique aims to treat anteroinferior glenohumeral instability by transferring the long head of the biceps through a subscapularis split to the anterior glenoid margin, thereby creating a “sling” and a “hammock” effect, similar to the ones achieved with the Latarjet procedure. This technique provides a more robust anterior stabilization when compared to the isolated Bankart repair, without the risks and complications classically associated with bone block procedures.
Nicolas Bonnevialle
Orthopedic Surgeon, CHU de Toulouse, France
Nothing beats Classic Latarjet
The Latarjet procedure is a widely used technique for treating anterior shoulder instability in patients with glenoid bone loss. In this lecture, Nicolas Bonnevialle highlights the advantages of the classic Latarjet method over modern variations. He discusses the biomechanical principles behind the procedure, including the triple locking effect, where the coracoid graft not only provides structural stability but also functional support through the subscapularis tendon.
Bonnevialle further examines the long-term outcomes of the classic technique, comparing clinical studies and patient results with alternative methods such as the arthroscopic Latarjet procedure. He emphasizes that the classic technique offers reliable fixation and lasting stability, allowing patients to undergo rapid functional rehabilitation with a low risk of complications.
The lecture concludes with a discussion on the optimal indications for the Latarjet procedure and the role of surgical experience in achieving the best results. Bonnevialle underscores that, despite technological advancements, the classic Latarjet method remains the gold standard for treating complex shoulder instability.
Wybren van der Wal
Orthopedic Surgeon, Ziekenhuis Gelderse Vallei, The Netherlands
Meniscus Root Injuries: Bridging Biomechanics with Modern Practice
Meniscus root injuries are increasingly recognized as a critical factor in knee joint degeneration, often leading to rapid cartilage deterioration and early osteoarthritis. In this lecture, Wybren van der Wal explores the biomechanical implications of meniscus root tears and the latest advancements in surgical repair techniques.
A key focus of the lecture is the role of the meniscus in load distribution, emphasizing how root injuries disrupt knee biomechanics, leading to increased tibiofemoral contact pressures. Van der Wal discusses modern surgical approaches, including transosseous root repair and suture anchor fixation, comparing their effectiveness in restoring meniscal function and joint stability.
The session also covers rehabilitation strategies, highlighting the importance of early mobilization, progressive loading, and neuromuscular training to optimize post-surgical recovery. Van der Wal presents clinical outcomesdemonstrating how timely intervention can significantly improve long-term knee health and delay the progression of osteoarthritis.
The lecture concludes with insights into future directions, including biological augmentation techniques, AI-driven surgical planning, and regenerative therapies aimed at enhancing meniscal healing and preservation. Van der Wal underscores that bridging biomechanics with modern surgical practice is essential for achieving optimal patient outcomes.
Alan Getgood
Orthopedic Surgeon, Aspetar, Qatar
The Role of Alignment in Meniscal Injury Treatment
Meniscal injuries are a common concern in orthopedic practice, often leading to pain, dysfunction, and an increased risk of osteoarthritis. In this lecture, Al Getgood explores the critical role of lower limb alignment in both the development and treatment of meniscal injuries. He discusses how malalignment, particularly in the medial compartment, contributes to excessive mechanical stress on the meniscus, accelerating degeneration and increasing the likelihood of injury.
A key focus of the lecture is the biomechanical relationship between axial alignment and meniscal pathology. Getgood examines how realignment osteotomy can serve as an effective strategy to off-load the affected knee compartment, thereby preserving meniscal integrity and delaying the progression of osteoarthritis. He outlines the indications for tibial and femoral osteotomy, depending on the location of the primary deformity, and presents evidence supporting the efficacy of these interventions in restoring knee function.
The lecture concludes with a discussion on surgical techniques, patient selection, and post-operative rehabilitation strategies to optimize outcomes. Getgood emphasizes that understanding the interplay between alignment and meniscal health is essential for developing comprehensive treatment plans that go beyond isolated meniscal repair
Andy Williams
Orthopedic Surgeon, Fortius Clinic, United Kingdom
Meniscus Injury in High Level Athletes
Meniscal injuries in elite athletes are a common cause of missed game time and even have the potential to be career shortening. In this patient group, care must be paid not only to the pathology, but also to a player’s contract status, time in the season, specific demands of his/her sport and position on the field, and future consequences. Successful treatment requires the clinician to understand the player’s goals and needs, communicate effectively between all stakeholders, and a have knowledge of the challenges posed by the different types of meniscal tear seen in this population.
Many meniscal tears are correctly treated non-operatively.
Paramount is the distinction between injuries to the medial and lateral meniscus. Deficiency of the lateral meniscus, as a result of a tear or a meniscectomy, leads to frequent early problems and inexorably to chondral degeneration thereby affecting an athlete’s ability to perform. Therefore, it is strongly recommended to repair the majority of lateral meniscal tears regardless of their severity. By happy co-incidence lateral meniscal tears are very favourable for healing due to the proximity of the inferior lateral meniscal artery.
Medial meniscal tears pose a more challenging treatment dilemma, as repair has poor results, whilst partial meniscectomy is reliable in achieving reproducible, early return to play, and only late osteoarthritis – often post-career. However, in the longer term osteoarthritis will occur. Nevertheless, in the majority of athletes medial meniscectomy is my first choice unless in athlete’s younger than 18 years of age, and fast-bowlers in cricket.
We have established that in elite athletes undergoing meniscal repair traditional in-out suturing technique is far superior to modern all-inside suturing for the medial meniscus at least.
Ewoud van Arkel
Orthopedic Surgeon, Haaglanden Medisch Centrum, The Netherlands
Meniscal Transplant, 25 years of Experience
Meniscal transplantation has evolved significantly over the past 25 years, offering a viable solution for patients suffering from irreparable meniscal damage. In this lecture, Ewoud van Arkel shares his extensive experience in performing meniscal transplants, highlighting the indications, surgical techniques, and long-term outcomes of the procedure.
Van Arkel discusses the biomechanical importance of the meniscus as a shock absorber in the knee joint and the consequences of meniscal loss, including pain, instability, and early osteoarthritis. He emphasizes the patient selection criteria, noting that age, knee stability, and cartilage condition play crucial roles in determining eligibility for transplantation.
The lecture explores the surgical advancements that have refined meniscal transplantation over the years, including graft fixation techniques and post-operative rehabilitation protocols. Van Arkel presents clinical data demonstrating the success rates of the procedure and its ability to restore knee function while delaying the need for joint replacement.
The session concludes with insights into the future of meniscal transplantation, including ongoing research into synthetic meniscal implants and biological augmentation strategies to enhance graft integration.
Enrico de Visser
Orthopedic Surgeon, CWZ, Nijmegen, The Netherlands
Hip Arthroscopy
Laurie Hiemstra
Orthopedic Surgeon, Banff Sport Medicine, Canada
Patellofemoral Instability Instability in the Setting of High-Grade Dysplasia: The Role of MPFL Reconstruction and Trochleoplasty
Patellofemoral instability in patients with high-grade trochlear dysplasia presents unique surgical challenges. In this lecture, Laurie Hiemstra explores the role of medial patellofemoral ligament (MPFL) reconstruction and trochleoplasty in restoring stability and improving patient outcomes. She discusses how isolated MPFL reconstructionoften fails in cases of severe dysplasia, necessitating a combined approach that addresses both soft tissue and bony abnormalities.
A key focus of the lecture is the thin flap trochleoplasty technique, which modifies the trochlear groove to enhance patellar tracking and reduce redislocation rates. Hiemstra presents clinical data demonstrating that trochleoplasty combined with MPFL reconstruction leads to significant improvements in patient-reported outcomes, including reduced apprehension, improved knee function, and lower rates of reoperation. She highlights the surgical indications, emphasizing that Dejour type B and D dysplasia with recurrent instability are prime candidates for this approach.
The lecture concludes with a discussion on post-operative rehabilitation, long-term success rates, and the evolving role of biomechanical assessments in refining treatment strategies. Hiemstra underscores that trochleoplasty, when performed in carefully selected patients, is a reliable and effective solution for persistent patellofemoral instability.
Rico Schuijers
Sports Psychologist, ProTask, Doornenburg, The Netherlands
Psychological Skills for Elite Performances and Mental Health
Elite athletes and high-performance professionals face immense psychological pressures that can impact both their performance and mental well-being. In this lecture, Rico Schuijers explores the essential psychological skills required to excel under pressure while maintaining mental resilience. He discusses how focus, confidence, and emotional regulation play a crucial role in achieving peak performance.
A key aspect of the lecture is the practical application of mental training techniques, including visualization, self-talk, and stress management strategies. Schuijers emphasizes that mental preparation is just as vital as physical training, and he presents evidence-based methods to enhance concentration, motivation, and recovery. He also addresses the psychological challenges faced by elite performers, such as performance anxiety, burnout, and the transition out of professional sports.
The session concludes with insights into mental health support systems, highlighting the importance of coaching, peer networks, and professional psychological guidance in sustaining long-term success. Schuijers underscores that mental strength is not innate but can be trained, making psychological skills an indispensable component of elite performance.
James Calder
Orthopedic Surgeon, Fortius Clinic, UK
Optimal Treatment for Navicular Fractures in Athletes
There has been a gradual evolution in the debate regarding the optimal treatment of navicular stress fractures. A 2010 meta-analysis by Torg et al. could find no advantage for operative treatment over non-weightbearing immobilization, although a high failure rate was reported with early weight-bearing.[i] However, more recent literature suggest that operative intervention may provide a more predictable outcome and return to sports for the professional athlete. Attia et al in a systematic review and meta-analysis comprised of 315 navicular stress fractures concluded that operative treatment was associated with a lower rate of re-fracture and non-union and a higher rate of success (96.3%) when compared with non-operative treatment (72.0%).[ii] Return to play rates upwards of 99% have been noted in those patients treated operatively, while time to return to play was just over 4 months in a further meta-analysis. Post-operative CT scans are frequently recommended to document healing of the fracture prior to allowing return to sport.
Percutaneous screw fixation is most commonly recommended for incomplete fractures with mini-open grafting of the fracture site and screw fixation in more complex and chronic cases.[iii] . Vascularised periosteal rotational flaps have been reported to have high rates of success for fracture non-unions, re-fractures and chronic cases with markedly sclerotic margins.[iv]
[i] Torg JS, Moyer J, Gaughan JP and Boden BP. Managemant of tarsal navicular stress fractures: conservative versus surgical treatment: a meta-analysis. Am J Sports Med. 2010 May; 38(5): 1048-53.
[ii] Attia AK, Mahmoud K, Bariteau J, Labib SA, DiGiovanni CW and D’Hooghe P. Return to sport following navicular stress fracture: a systematic review and meta-analysis of three hindred and fifteen fractures. Int Orthop. 2021 Oct; 45(10): 2699-710.
[iii] Gross CE and Nunley JA. Navicular stress fractures. Foot Ankle Int. 2015 Sep; 36(9): 1117-22.
[iv] Nunley JA, Green C, Morash J and Easley ME. Treatment of navicular stress fractures with an algorithmic approach. Foot Ankle Int. 2022 Jan; 43(1): 12-20.
Ursula Zdanowicz
Orthopedic Surgeon, Carolina Medical Center, Pittsburgh, USA
Operative Reconstruction of Lateral Ankle Ligaments
Chronic lateral ankle instability is a common issue among athletes and active individuals, often requiring surgical intervention when conservative treatments fail. In this lecture, Ursula Zdanowicz explores the latest advancements in operative reconstruction techniques for restoring ankle stability and function.
A key focus of the lecture is the anatomical and biomechanical considerations in ligament reconstruction, particularly the role of the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) in maintaining lateral ankle stability. Zdanowicz discusses the indications for primary repair versus reconstruction, comparing autograft, allograft, and synthetic ligament options for optimal outcomes.
The session also covers minimally invasive techniques, including arthroscopic-assisted ligament repair, which has shown promising results in reducing recovery time and improving post-operative mobility. Zdanowicz presents clinical data on functional outcomes, complication rates, and return-to-sport timelines, emphasizing the importance of individualized treatment planning based on patient-specific factors.
The lecture concludes with insights into post-operative rehabilitation, highlighting strategies to enhance proprioception, neuromuscular control, and long-term joint stability. Zdanowicz underscores that advancements in surgical techniques and rehabilitation protocols continue to improve patient outcomes, making operative reconstruction a reliable solution for persistent lateral ankle instability.
Sjoerd Stufkens
Orthopedic Surgeon, Amsterdam UMC, The Netherlands
Orthopaedic medicine; hormones, habits, pain and psychology
Orthopedic conditions are often viewed through a purely mechanical lens, but hormonal influences, behavioral habits, pain perception, and psychological factors play a crucial role in musculoskeletal health. In this lecture, Sjoerd Stufkens explores the multifaceted relationship between these elements and their impact on injury recovery, chronic pain, and surgical outcomes.
A key focus of the lecture is the interaction between hormones and musculoskeletal function, including the effects of cortisol, estrogen, and testosterone on bone density, ligament integrity, and healing processes. Stufkens discusses how stress and hormonal imbalances can contribute to delayed recovery and increased pain sensitivity, emphasizing the need for a holistic approach to orthopedic treatment.
The session also examines habit formation and behavioral patterns that influence injury prevention and rehabilitation. Stufkens highlights the role of movement psychology, patient adherence to therapy, and the impact of chronic pain on mental health, presenting strategies to optimize long-term musculoskeletal well-being.
The lecture concludes with insights into integrative treatment approaches, including psychological interventions, lifestyle modifications, and personalized rehabilitation protocols. Stufkens underscores that orthopedic medicine must evolve beyond structural repair, incorporating biological and psychological factors to enhance patient outcomes.
Roger van Riet
Orthopedic Surgeon, AZ Monica, Antwerp, BE
The Elbow
The elbow joint is a complex structure that plays a crucial role in upper limb function, yet it is often overlooked in orthopedic discussions. In this lecture, Roger van Riet, a world-renowned elbow surgeon, explores the biomechanics, pathology, and surgical management of elbow conditions, emphasizing the latest advancements in arthroscopic and reconstructive techniques.
A key focus of the lecture is the treatment of elbow instability, particularly in athletes and individuals with ligamentous injuries. Van Riet discusses his pioneering work in arthroscopic surgery, highlighting minimally invasive approaches to repair and reconstruct unstable elbows. He presents clinical data on tendon repairs, fracture management, and post-traumatic stiffness, offering insights into optimizing patient outcomes.
The session also covers elbow prosthesis development, an area where Van Riet has contributed significantly. He examines the indications for joint replacement, comparing different implant designs and their impact on function and longevity.
The lecture concludes with a discussion on rehabilitation strategies, emphasizing the importance of early mobilization, neuromuscular training, and patient-specific recovery protocols. Van Riet underscores that advancements in elbow surgery continue to improve outcomes, making specialized treatment essential for complex cases.
Paul Koning
Orthopedic Surgeon n.p., Co-Founder OurMind, The Netherlands
AI in Orthopedics
Artificial intelligence is rapidly transforming the field of orthopedics, offering new possibilities for diagnostics, surgical planning, and patient care. In this lecture, Paul Koning, co-founder of OurMind, explores the evolving role of AI-driven technologies in orthopedic practice, emphasizing their potential to enhance efficiency, accuracy, and decision-making.
A key focus of the lecture is the integration of AI in clinical workflows, including automated image analysis, predictive modeling for surgical outcomes, and AI-assisted triage systems. Koning discusses how AI can support orthopedic surgeons by reducing administrative burdens, improving patient consultations, and optimizing treatment strategies. He highlights OurMind’s approach to personal AI assistants, designed to help healthcare professionals streamline their work and improve doctor-patient interactions.
The session also covers ethical considerations, addressing concerns about data privacy, algorithm bias, and the balance between AI automation and human expertise. Koning presents real-world applications of AI in orthopedic surgery, showcasing how AI-powered tools are already making an impact in preoperative planning, rehabilitation monitoring, and clinical decision support.
The lecture concludes with insights into the future of AI in orthopedics, including advancements in machine learning, robotics, and personalized medicine. Koning underscores that AI is not replacing surgeons but augmenting their capabilities, enabling more precise, efficient, and patient-centered care.
Alan Getgood
Orthopedic surgeon, Doha, Qatar
&
Andy Williams
Orthopedic surgeon, Fortius Clinic, UK
Advanced approaches to multi-ligament knee injuries and meniscus preservation
Stefan Heijnen
Orthopedic surgeon, Bergman clinics, The Netherlands
&
Yde Engelsma
Orthopedic surgeon, Bergman clinics, The Netherlands
“Preserve the Knee, Repair the Meniscus “ Live Surgery & Expert Insights.
Rintje Agricola
Orthopedic Surgeon, Anna Ziekenhuis, The Netherlands
&
Tom Beddows
PhD Erasmus MC, Rotterdam, The Netherlands
The Female Athlete: From Hip Morphology to Osteoarthritis (PROFE Study)
Female athletes experience unique hip morphology variations that may predispose them to early osteoarthritis (OA). In this lecture, Agricola and Beddows explore the PROFE Study, which investigates the relationship between hip structure, biomechanics, and OA development in female athletes. They discuss how sport-specific loading patternsinfluence hip joint adaptation, potentially leading to femoroacetabular impingement (FAI) and cartilage degeneration.
A key focus of the lecture is the longitudinal analysis of hip morphology changes over time, examining how training intensity, movement mechanics, and genetic predisposition contribute to OA risk. The speakers present findings from prospective cohort studies, highlighting early detection strategies and preventative interventions to mitigate long-term joint damage.
The session also covers clinical implications, including diagnostic imaging techniques, biomechanical assessments, and targeted rehabilitation protocols for female athletes at risk of OA. Agricola and Beddows emphasize the importance of personalized treatment approaches, integrating sports medicine, orthopedic surgery, and physiotherapy to optimize hip health.
Hiske Kneepkens
Sportsmed, NOCNSF, The Netherlands
Paralympic Power: The Team Behind the Athlete
Elite Paralympic athletes achieve extraordinary performances, but behind every success is a dedicated multidisciplinary team ensuring optimal physical and mental preparation. In this lecture, Hiske Kneepkens, a leading sports physicianspecializing in Paralympic sports, explores the high-performance support systems that enable athletes to compete at the highest level.
A key focus of the lecture is the collaboration between sports medicine, rehabilitation specialists, and performance coaches, highlighting how injury prevention, recovery strategies, and adaptive training are tailored to each athlete’s unique needs. Kneepkens discusses the importance of medical innovation, including prosthetic advancements, neuromuscular therapies, and personalized conditioning programs, which play a crucial role in maximizing performance.
The session also covers the psychological resilience required for Paralympic competition, emphasizing the role of mental coaching, stress management, and motivation techniques in sustaining elite performance. Kneepkens presents case studies demonstrating how integrated medical and coaching teams contribute to long-term athletic success.
The lecture concludes with insights into future developments in Paralympic sports medicine, including cutting-edge rehabilitation technologies, AI-driven performance analytics, and enhanced athlete support networks. Kneepkens underscores that behind every Paralympic champion is a team of experts working tirelessly to optimize their journey.
Laurie Hiemstra
Orthopedic Surgeon, Banff Sport Medicine, Canada
Examination and Rehabilitation Considerations of Patients with Patellofemoral Instability – not just your Standard Knee Evaluation
Patellofemoral instability presents unique challenges in diagnosis, treatment, and rehabilitation, requiring a comprehensive evaluation beyond standard knee assessments. In this lecture, Laurie Hiemstra explores the multifactorial nature of patellofemoral instability, emphasizing the importance of biomechanical, anatomical, and neuromuscular factors in guiding treatment decisions.
A key focus of the lecture is the Banff Patellofemoral Instability Instrument (BPII), a validated patient-reported outcome measure designed specifically for assessing quality of life in patients with patellar instability. Hiemstra discusses how traditional knee evaluations often overlook psychosocial and functional impairments, leading to suboptimal treatment strategies. She highlights the importance of individualized rehabilitation protocols, incorporating neuromuscular training, proprioceptive exercises, and movement retraining to enhance long-term stability and function.
The session also covers surgical considerations, including MPFL reconstruction, trochleoplasty, and tibial tubercle osteotomy, with insights into post-operative rehabilitation tailored to patellofemoral biomechanics. Hiemstra presents clinical data demonstrating how targeted rehabilitation strategies improve patient outcomes and reduce recurrence rates.
The lecture concludes with a discussion on future directions, including AI-driven movement analysis, personalized rehabilitation algorithms, and advancements in surgical techniques to optimize patellofemoral stability. Hiemstra underscores that effective management of patellofemoral instability requires a holistic approach, integrating clinical expertise, patient-reported outcomes, and biomechanical insights.
Jiri Rutten
Physiotherapist and Manual Therapist, Fysiotherapie Utrecht, The Netherlands
Patients with Patellofemoral instability, get ‘em stable on the field!
Patellofemoral instability is a complex challenge for athletes, often leading to recurrent dislocations, pain, and functional limitations. In this lecture, Jiri Rutten, an expert in sports physiotherapy and manual therapy, explores evidence-based strategies to restore stability and performance for athletes dealing with patellofemoral instability.
A key focus of the lecture is the biomechanical assessment of instability, emphasizing the importance of movement analysis, neuromuscular control, and kinetic chain influences. Rutten discusses functional rehabilitation techniques, including proprioceptive training, dynamic stabilization exercises, and sport-specific movement retraining, to help athletes regain confidence and control on the field.
The session also covers return-to-sport protocols, highlighting progressive loading strategies, plyometric drills, and individualized rehabilitation plans to ensure safe and effective reintegration into competitive play. Rutten presents case studies demonstrating how targeted interventions can significantly reduce re-injury risk and enhance long-term knee stability.
The lecture concludes with insights into collaborative approaches, emphasizing the role of physiotherapists, orthopedic specialists, and strength coaches in optimizing athlete recovery and performance. Rutten underscores that patellofemoral instability requires a proactive, multidisciplinary approach, ensuring athletes can return to peak performance with confidence.
Alan Getgood
Orthopedic Surgeon, Aspetar Qatar
Individualized ACL Reconstruction – Lessons from the Stability Trials
Anterior cruciate ligament (ACL) reconstruction has evolved significantly, with individualized surgical approachesplaying a crucial role in optimizing patient outcomes. In this lecture, Al Getgood explores key findings from the Stability Trials, which investigate the effectiveness of lateral extra-articular tenodesis (LET) in ACL reconstruction for high-risk patients.
A key focus of the lecture is the biomechanical rationale behind LET augmentation, examining how additional lateral stabilization can reduce rotational instability and improve graft survival rates. Getgood presents clinical data demonstrating that young, active individuals—particularly those involved in pivoting sports—benefit from combined ACL reconstruction and LET, leading to lower re-injury rates and enhanced functional recovery.
The session also covers patient selection criteria, highlighting factors such as ligamentous laxity, pivot shift severity, and knee morphology that influence surgical decision-making. Getgood discusses long-term follow-up results, emphasizing the importance of individualized treatment planning to optimize return-to-sport outcomes.
The lecture concludes with insights into future directions, including AI-driven surgical planning, advanced graft selection techniques, and personalized rehabilitation protocols. Getgood underscores that ACL reconstruction is not a one-size-fits-all procedure, and tailoring surgical approaches to patient-specific risk factors is essential for achieving durable knee stability.
Andy Williams
Orthopedic Surgeon, Fortius Clinic, United Kingdom
MCL Anatomy, and Biomechanics, and their Relevance to MCL Surgery
Introduction
The medial collateral ligament (MCL) is the most commonly injured knee ligament. The MCL complex has a large surface area and good blood supply with excellent healing potential following injury, which means many injuries can be managed non-operatively. However, there is growing recognition that not all MCL injuries are benign nor should all MCL lesions be treated non-operatively.
Anatomy and Biomechanics
The MCL complex is an arrangement of three structures within separate layers of tissue: layer 1- deep investing fascia; layer 2- includes the superficial MCL (sMCL), and layer 3- the capsule, deep MCL (dMCL) and the posterior oblique ligament (POL) / posteromedial capsule (PMC). The sMCL is often described to attach posterior to the medial epicondyle, but our work suggests it is concentrated on the epicondyle itself. The dMCL has been regarded as a capsular thickening sited immediately deep to the superficial MCL. However, our recent work suggests that the dMCL has an inverted fan-like structure attaching to the femur distal and posterior to the femoral attachment of the sMCL. The fibres pass anterodistally and have a broad tibial insertion close to the joint line and is well aligned to resist anterior translation of the medial tibia/external rotation.
There is unanimous agreement that the sMCL is the primary restraint to valgus load throughout range of motion. While it was previously thought that the sMCL was responsible for resisting tibial external rotation, our studies and those of others suggest that the dMCL is the primary restraint to tibial external rotation across 0-30 degrees flexion and the sMCL is only the primary restraint above 90 degrees (there is load sharing 30-90 degrees). This accounts for the occurrence of an unusual isolated dMCL lesion most commonly seen in professional soccer players and underlines the dMCL is actually very important. If adequate healing is not achieved persistent laxity can result in anteromedial rotatory instability, which in turn increases the risk of ACL injury. There is therefore a need to appreciate and understand the injury “completely” and to have surgical techniques that enable stability to be achieved.
Anteromedial Rotatory Instability
The concept of anterolateral rotatory instability has again been popularized recently and led to resurgence of lateral extra-articular procedures to de-stress an ACL graft. Whilst there has been a lot of interest in this field, anteromedial rotatory instability (AMRI) has been rather neglected. Cadaveric studies show increased ACL tension with applied external rotation torque with MCL laxity. There are now clinical studies which confirm unaddressed medial laxity is associated with increased ACL graft failure.
MCL surgery
Whilst the majority of MCL injuries, whether isolated or in combination with other ligaments, can be treated satisfactorily with non-operative means, there are clear scenarios where surgical intervention is advised.
In cases with chronic laxity with instability there is clearly a need for surgery, as there is no healing potential. In the acute phase, there is healing potential, hence the decision to operate is more difficult. Surgery should be considered when adequate healing is not expected. We suggest surgery in cases of valgus laxity of the knee in full extension; grade 3 laxity; a positive dial test for anteromedial rotation; a tibial sided injury with a ‘Stener’ lesion or an in-folding of the ligament into the joint; and when combined with ACL rupture with a positive Slocum test (i.e. persistence of the anterior drawer to test laxity despite external rotation) and / or grade 2 MCL laxity in athletes. It is only a minority of cases that need surgery.
Surgical Techniques
There are many procedures described for MCL reconstruction and most of them include components for the POL and sMCL, but ignore the dMCL. It seems particularly strange that when addressing anteromedial rotatory instability, which is a result of injuries to the ACL and the medial structures, a component for the POL is even considered at all. The POL passes in the opposite direction to the ACL, as opposed to the dMCL which runs parallel to the ACL!
In acute cases that require surgery, repair of the damaged structures is desirable. Restoration of natural anatomy is superior to reconstruction alone as it allows normal function of the soft tissue elements of the MCL and is more likely to restore proprioceptive feedback from the ligament complex. Whilst simple suture repair of the acutely injured soft tissues maybe sufficient on its own, I believe in the concept of protecting the acute repair with reconstructive surgery in most cases. In chronic cases suture techniques should be used to restore anatomy at the right tensions and these too should be protected with reconstruction- grafts alone can never ‘be’ the MCL!
Reconstruction Techniques
Most reconstruction techniques use soft tissue grafts to reproduce the sMCL and the POL. Our studies show this concept does not control external rotation. New approaches to MCL reconstruction have been described based on the recent concepts of anatomy and biomechanics described above. These techniques include grafts for dMCL and sMCL but not the POL when using them to treat anteromedial rotatory instability with ACL deficiency. For many years, I have undertaken a single strand reconstruction with the proximal end of the graft attached to the centre of the epicondyle of the femur and the distal end 2cm distal to the joint line. The advantage is that the short graft may stretch less than a longer one and that the site of proximal tibial attachment is proximal to the pes anserinus, thereby avoiding soft tissue irritation and enjoying better quality bone than more distal fixation allows. In addition, a short graft will provide rotational restraint too. This technique has recently been shown to be effective in our laboratory.
Conclusion
In view of more recent publications of anatomy, biomechanics, and surgical technique, the MCL needs to be assessed very carefully when acutely injured as an isolated injury or particularly in combination with other ligaments such as the ACL. The MCL is the most commonly injured ligament in a knee and whilst the majority of cases do well without surgery, a significant minority require it. Appreciation of the basic science and application of this with more appropriate reconstructive surgery and repair is likely to improve the outcome of not only MCL reconstruction but will reduce ACL graft re-rupture.
Marc Jacob Strauss
Orthopedic Surgeon, Oslo University Hospital, Ullevål, Norway
ACL Revisions, One- or Two-Stage, with or without Lateral Extra-articular Procedure.
Revision ACL reconstruction presents unique challenges, requiring careful surgical planning to optimize outcomes. In this lecture, Marc Jacob Strauss explores the decision-making process behind one-stage vs. two-stage revision ACL surgery, as well as the role of lateral extra-articular procedures in improving knee stability.
A key focus of the lecture is the biomechanical rationale for lateral extra-articular augmentation, particularly in cases of persistent rotational instability. Strauss discusses findings from recent studies, which indicate that adding a lateral extra-articular procedure to revision ACL reconstruction significantly reduces failure rates without increasing complications. He examines the indications for isolated intra-articular revision vs. combined procedures, highlighting patient-specific factors such as pivot shift severity, tunnel widening, and ligamentous laxity.
The session also covers technical considerations, including graft selection, fixation methods, and rehabilitation protocols tailored to revision ACL surgery. Strauss presents clinical data comparing outcomes of one-stage vs. two-stage revisions, emphasizing that two-stage procedures are particularly beneficial in cases of severe tunnel widening or concomitant knee pathology.
The lecture concludes with insights into future advancements, including AI-assisted surgical planning, improved graft integration techniques, and personalized rehabilitation strategies. Strauss underscores that individualized treatment approaches are essential for achieving long-term knee stability and optimal functional recovery.
Het is helaas niet meer mogelijk om een abstract in te dienen. De termijn liep tot 1 juli 2025. De gelukkigen zijn hier van op de hoogte gesteld.
De wetenschappelijke commissie selecteert 5 abstracts voor een mondelinge presentatie. Deze sprekers dingen mee naar de Dr. Harry Eikelaar prijs van € 3000 en “de Gouden Eikel – wisseltroffee voor de beste presentatie / het beste abstract.
De prijs wordt aan het einde van de dag uitgereikt.
Locatie
Het Lustrum Congres 2025 vindt plaats bij:
Grand Hotel Huis ter Duin
Koningin Astrid Boulevard 5 te Noordwijk
Registratie tarieven:
| Voordelige package deal – hotelkamer enkel gebruik:
(2 dgn congres, 1 nacht hotel – enkel gebruik, 1 kaartje feest) |
|
| NVA lid – Package deal | 750 |
| A(N)IOS lid – Package deal | 550 |
| Niet NVA lid – package deal | 850 |
| Voordelige package deal – gedeelde kamer:
(2 dgn congres, 1 nacht hotel (gedeelde kamer), 1 kaartje feest) |
|
| NVA lid – Package deal | 650 |
| A(N)IOS lid – Package deal | 450 |
| Niet NVA lid – package deal | 750 |
| Nee, ik wil geen package deal | |
| NVA lid 1 congresdag | 250 |
| NVA lid 2 congresdagen | 475 |
| A(N)IOS lid 1 congresdag | 125 |
| A(N)IOS lid 2 congresdagen | 225 |
| Geen lid 1 congresdag | 300 |
| Geen lid 2 congresdagen | 575 |
| Kaartje feestavond | 90 |
Inschrijven
Promotie actie – Bring Your Own Sportsmed / Sportsfysio
Kent u of werkt u samen met een sportmedische arts of fysiotherapeut die dit ook niet wil missen? Introduceer deze persoon en ontvang beiden €50,- korting op de tickets. Hoe werkt dit? Schrijf u beiden in voor het congres, voeg de naam van deze persoon toe bij de daarvoor bestemde vraag. Gebruik de kortingscode: promonva25 in het kopje vóór betaling. Zo kunnen jullie dit samen beleven!
Voor de registratie-tarieven kijkt u hier:
Sponsoring
Dit event wordt mede mogelijk gemaakt door financiële ondersteuning, oftewel sponsoring door farmaceutische- en of hulpmiddelen- leveranciers.
De deelnemende sponsoren hebben geen enkel invloed op het programma.
Dit event wordt gehouden aan de CGR– en/of de GMH– wet- en regelgeving en sponsoring wordt openbaar gemaakt in het TRZ-Transparantieregister Zorg.
Als zorgprofessional moet je onafhankelijk kunnen werken, hier: Hoeblijfikonafhankelijk.nl vindt u alle informatie ter voorkoming van belangenverstrengeling.
Van alle deelnemers van dit event, zoals; de opdrachtgever, de organisator, de sponsor, de dienstverlener en de zorgprofessional/ beroepsbeoefenaar wordt verwacht om transparant te zijn over de financiële relaties.
Interesse in sponsoring? Neem contact op met info@excelcs.nl.
